The aim of this research group is to understand the mechanisms underlying the role of the limbal epithelial stem cells in corneal avascularity. Specifically, we are interested in the effect of UV irradiation on the limbal stem cell phenotype and pathological neovascularisation.
Vision is a key sensory function. Clear vision depends on transparency of the structures of the visual axis. Consequently, normal corneal tissue (the “windscreen of the eye”) is in an avascular and low inflammatory state. The limbal epithelial stem cells (LESC) maintain the integrity of the corneal epithelium thus preventing neovascularization, stromal scarring and conjunctivalisation. Although it has been proven both clinically and experimentally that LESCs destruction compromises corneal avascularity, the exact mechanisms by which this is achieved remain unidentified.
Our group focuses on elucidating these mechanisms and aims to identify new LESC-related regulators of corneal neovascularisation which will lead to new therapeutic options (we are part of FOR2240, “(Lymph)angiogenesis and cellular immunity in inflammatory diseases of the eye”). Exposure to UV irradiation compromises the LESC niche and induces corneal (lymph)angiogenesis. Pterygium, a non-cancerous tumour of the conjunctiva, is linked to UV-induced DNA and oxidative damage. The phenotype is associated with inflammation and neovascularisation causing discomfort and decrease of vision.
Preliminary evidence links pterygium onset to limbal epithelial stem cell (LESC) deficiency and own data suggest that following short term UV irradiation LESC become differentiated. However, a direct involvement of LESC DNA damage in the disease is not fully explored.
Our hypothesis is, that following UV-induced damage the inability of LESCs to repair DNA damage contributes to induction of pterygia. In collaboration with the laboratory of Professor Björn Schumacher we will aim to investigate the possible links between UV damage and neovascularization using a nucleotide excision repair deficient mouse model. We will investigate the association of ERCC1 with pterygium and the possibility of using the ERCC deficient mouse as a model for UV-induced alterations relevant to pterygium.
Also, we will explore the role of photolyase, a DNA repairing enzyme, as a therapeutic approach to prevent UV induced LESC damage leading to neovascularization, inflammation and thus pterygium.
Pterygium has a higher prevalence in countries with elevated ultraviolet exposure. It is estimated that an expected 10% of all refugees who came to Germany from southern countries will most likely suffer from pterygium (i.e.>100000), resulting in a significant burden to the health system. Therefore, understanding the mechanisms underlying the disease will help developing more efficient prevention and treatment strategies.
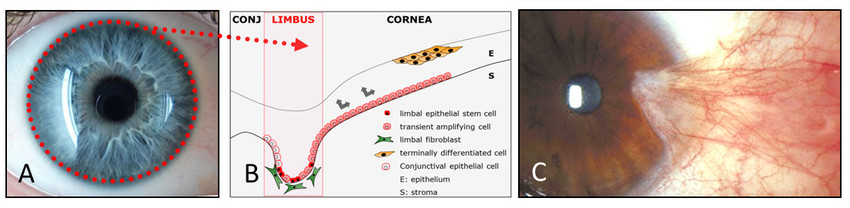
The corneal epithelium is maintained by a population of stem cells which reside at the limbus creating a border between the vascularised conjunctiva and the avascular cornea (A. noted in dotted line).
These limbal epithelial stem cells (LESC) migrate and proliferate to replace the epithelium which is lost due to injury, disease or normal ware and tare (B).
Pterygium, a UV-induced fibroblascular tumour of the conjunctiva, is an example where the limbal border is broken down allowing for the encroaching of blood and lymphatic vessels on the cornea (C).

Clinic of General Ophthalmology
CMMC - PI - CAP 15
show more…+49 221 478 30621
+49 221 478 32785
Clinic of General Ophthalmology
Kerpener Str. 62
50931 Köln
https://augenklinik.uk-koeln.de/forschung/zentrum-fuer-molekulare-medizin-koeln-zmmk/
Berbang Meshko (PhD Student)
Isabella Moshiri (GEROK Clinician Scientist)
Stephanie Brosig (Technician)
Marieke Dombey (Alumni - Master’s student)